Adjunctive Interventions
Implementation Change Methods
In implementation research and practice, one is often trying to simultaneously change the behaviors or conditions of multiple people (e.g., patients/clients, clinicians/providers, managers/leaders) using various types of change methods (e.g., education, support, infrastructure creation, policy change). Accurately attributing different functions and effects to the right change methods is critical to understanding a project’s successes and areas for adjustment.
There are three types of changes methods that we differentiate based on their intended targets, desired outcomes, and theory of action.
1. Health interventions are clinical, behavioral, or biomedical innovations designed to directly improve recipients’ (patients/clients) health outcomes (e.g., prevent disease occurrence, reduce severity of disease, improve quality of life).
2. Implementation strategies are actions taken to improve utilization of an intervention at the health system or provider level (e.g., policy change to improve reimbursement, provider training, provider audit and feedback, and colocation of services).
3. Adjunctive interventions are change methods that target recipients of a health intervention and designed to increase their motivation, self-efficacy, or capacity for initiating, adhering to, or engaging with the health intervention initially (i.e., uptake) and over time (i.e., adherence). Adjunctive interventions enhance recipients’ attitudes and behaviors towards utilizing a health intervention but have no direct causal link to health status. Thus, they are supplemental: not always necessary and never sufficient to achieve a health outcome.
Why are adjunctive interventions important? An examples from COVID.
Efforts to mitigate the COVID-19 pandemic with vaccines highlight the need to think about adjunctive interventions. The SARS-CoV-2 coronavirus vaccine is the health intervention because it directly prevents COVID-19 illness in patients. In the US, implementation strategies to scale up vaccination focused on facilitating recipient’s access via offering vaccinations at typical healthcare locations staffed by nurses (e.g., primary and urgent care), pharmacies, public health departments, community-based organizations, and other entities (e.g., churches). Financial strategies were also invoked by federal and local governments to eliminate cost-related barriers to recipients, and dissemination strategies were deployed to educate clinicians and the public about vaccine safety and effectiveness.
However, as of May 10, 2023, only 81% of the population had received at least one dose, and 70% were fully vaccinated (one or two doses). The below-target vaccination rates were not due to lack of availability for the vast majority of Americans, as evidenced by only 68% of distributed doses being administered; rather, individual uptake of vaccines was insufficient due to stigma, hesitancy, and misinformation, resulting in the majority of unused vaccines expiring (estimated 1.1 billion doses globally). Adjunctive interventions were needed to motivate and capacitate eligible people to use them.
Adjunctive interventions in HIV have not been well specified
Examples in HIV
– Patient education about PrEP
– Peer navigation for ART
– Financial incentives for getting an HIV test
– Motivational interviewing and counseling for medication adherence
– Digital HIV programs (e.g., text messaging, smartphone apps)
In our experiences reviewing the HIV implementation science literature and supporting EHE projects, misspecification consistently creates scientific problems:
When adjunctive interventions are treated as health interventions, the causal logic to health outcomes fails. No number of adjunctive interventions, in the absence of PrEP or ART, will change viral protection or suppression.
When adjunctive interventions are treated as implementation strategies, the causal logic to implementation determinants and implementation outcomes fails because adjunctive interventions do not target the health delivery system. Additionally, other strategies are needed to implement adjunctive interventions but are missing entirely.
The same change method is classified as an intervention in some studies and as a strategy in others. This inconsistency makes comparing and synthesizing across studies difficult.
Resources to differentiate change methods
Characteristics table
This table compares the three change methods to highlight similarities and differences.
| Characteristics | Clinical / Preventive / Health Intervention | Adjunctive Intervention | Implementation Strategy |
| Target | Directly influences recipients’ disease / condition outcomes of interest | Influences recipient behaviors and may be needed to enable interaction with the intervention | Influences implementer behaviors or the implementing system operations |
| Primary Outcomes | Symptoms, biomarkers, infection, diagnosis, other health outcomes | Recipient acceptability, uptake, utilization, adherence, completion, maintenance of the intervention | Implementer adoption, reach, feasibility, fidelity, sustainment of the intervention |
| Actions and Causal Processes |
Changes targets of disease / condition among recipients Direct, proximal cause of change to the endpoint health outcome |
Changes recipients’ behavior / motivation / access to and/or enhances / facilitates engagement with the intervention Distally impacts endpoint health outcome through receipt, adherence, and/or maintenance of the intervention; inert on its own |
Changes the way services and interventions are carried out as a result of implementer actions or system changes Inert on endpoint health outcome; requires the health intervention to have impact |
| Hierarchy /Level |
Requires the use of implementation strategies (delivered by implementers in a delivery system) Effects for some recipients can be enhanced by adjunctive interventions |
Requires the use of implementation strategies to support delivery May be indicated for only a subset of health intervention recipients |
Supports the implementation of either/both the health intervention and the adjunctive intervention |
| Indications | Biomarkers / health indicators / risk assessment | Innovation determinants (client-level barriers / facilitators) | Implementation determinants (system-level barriers / facilitators) |
Decision tree
This decision tree helps you identify whether a particular change method is a health intervention, implementation strategy, or adjunctive intervention.
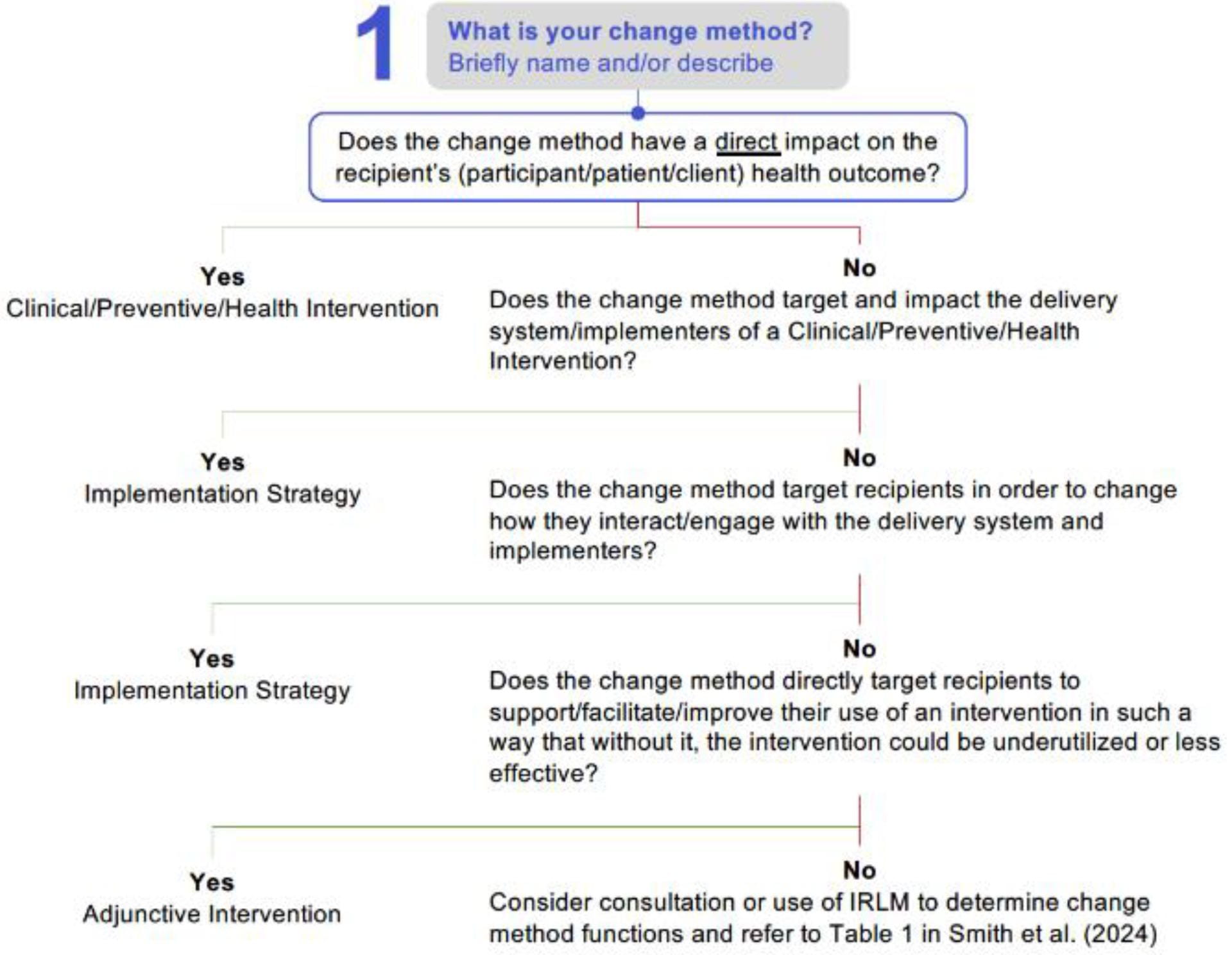
An accessible text version of the decision tree will be available soon.
Adaptation to the Implementation Research Logic Model
The Implementation Research Logic Model helps combine and organize implementation science frameworks; specify the relationships between constructs across frameworks; and improve the rigor, reproducibility, and transparency of a project. This modification to the IRLM includes space for adjunctive interventions and strategies for those adjunctive interventions.
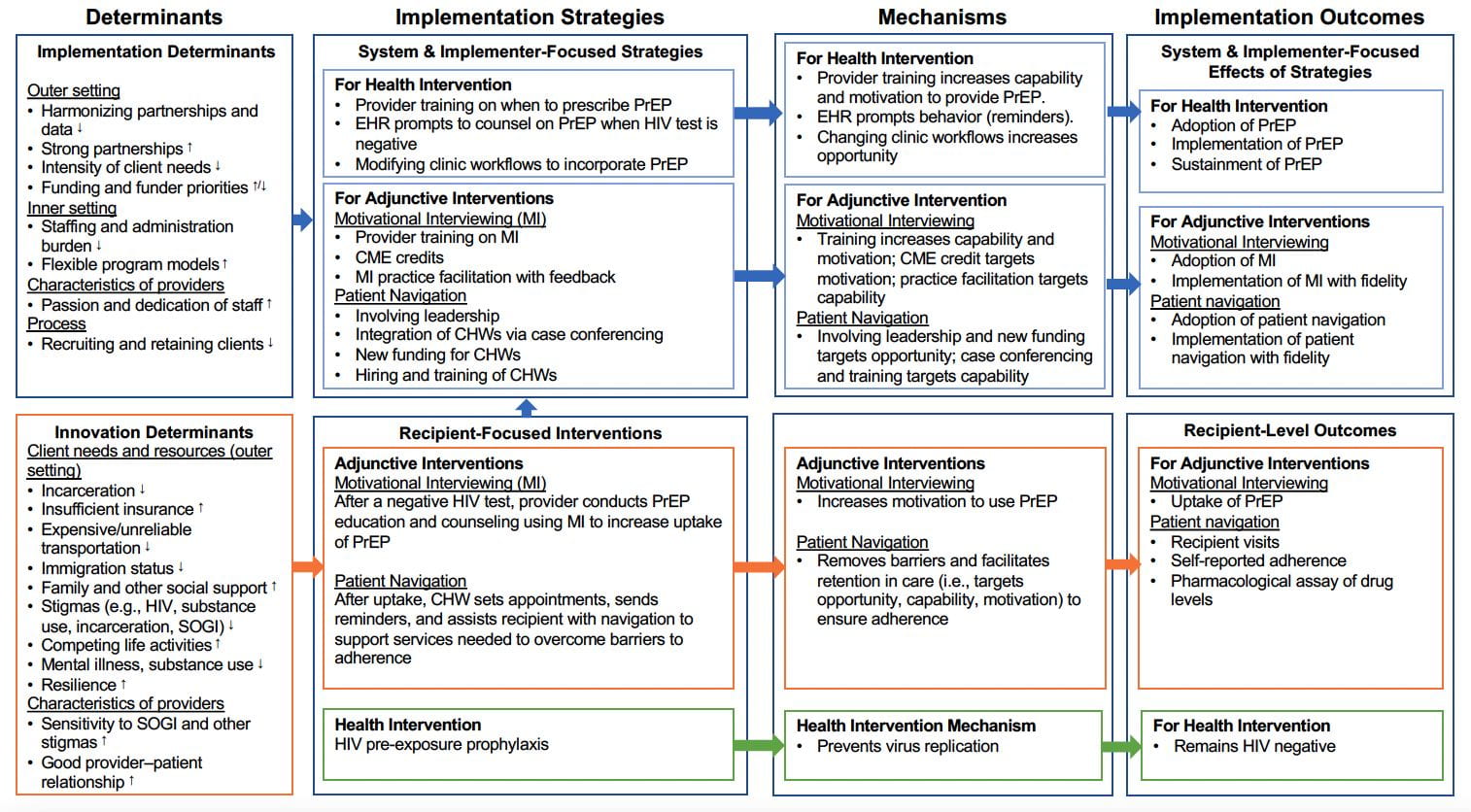
View this Adaptation to the Implementation Research Logic Model as a PDF.
